The Effects and Symptoms Caused by COVID
Why are COVID-19 symptoms so severe in some patients?
Since the beginning of the COVID-19 outbreak, scientists have been researching how the virus affects the body. In an article published in the Medical Hypotheses journal, Dr. Ashutosh Kumar suggests that some symptoms associated with COVID-19 are due to damage in blood vessels around the body.
COVID-19 is a disease caused by a virus, SARS-CoV-2. The SARS-CoV-2 virus is transmitted by droplets in the air that are inhaled through the nose and mouth. When SARS-CoV-2 enters the body, it binds to ACE2 receptors inside. These receptors are found on organs all over the body, and are especially concentrated in the nose, blood vessels, lungs, brainstem, and heart. In the blood vessels, they play a role in how large or small the vessels are, which can affect how fast blood pumps through the body. When the virus binds to these receptors, it can lead to damage within and near the affected site. The effects and symptoms seen with COVID-19 infection can be traced through the body where ACE2 receptors are present.
Receptor Binding

Receptors are like doors with locks that sit in the cellular membranes. These membranes can have many receptors, like a house with many doors. The right molecule must attach to the receptor to open it, like a key, and these molecules bounce around in the body until they find a receptor that they match with. This molecule allows other things to move into or out of the cell. The SARS-CoV-2 virus has very similar properties to the molecule that usually binds to the ACE2 receptor and binds allosterically to the receptor. Allosteric binding means that SARS-CoV-2 binds to the same place on the receptor as the normal molecule and can act like a piece of gum stuck in the lock for the ACE2 receptor. When the virus binds to the receptor as seen in figure 1, the ACE2 receptor cannot perform its normal functions and is downregulated or removed from the membrane, which leads to illness in the cell.
The first contact the virus has with the body is usually in the nose where many ACE2 receptors are located. When the virus affects these receptors, a patient can experience loss of taste and smell, some of the first signs of COVID-19 infection. The next location of infection is usually the lungs. As the virus gets deeper into the lungs where ACE2 receptors are located, it can damage the lungs and therefore make it harder to breathe. When the virus encounters the alveoli, small air sacs in the lungs that help transport oxygen to the capillaries, it irritates front line cells, inviting white blood cells to the area and causing inflammation in the lungs, as seen in figure2. As the white blood cells target and kill the cells that the virus has infected, they leave behind a mix of fluid and dead cells. This fluid is also the underlying symptom for pneumonia, a common disease that can occur with COVID-19 infection. Red blood cells from the heart usually pick up oxygen from the lungs and move it around the body to cells that need it. When the lungs are damaged and a patient is breathing in less oxygen, there is less oxygen available to move around the body. As a result, cells cannot get the energy they need to function and begin to get sick, leading to inflammation in other organs.


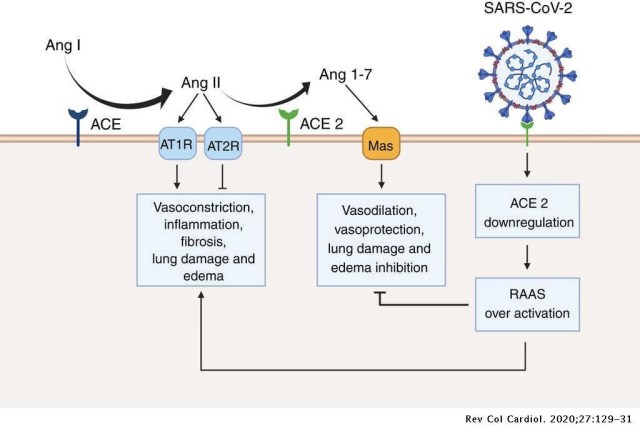
Sometimes a molecule attaches to a receptor and causes a change to something else inside of the cell. In the case of the ACE2 receptor, when the right molecule binds, it converts a hormone called angiotensin-II into a hormone called angiotensin(1-7). This is important because angiotensin-II is a vasoconstrictor, meaning it makes blood vessels smaller to allow blood to pump through the body faster. However, too much angiotensin-II can cause blood vessels to get too small, leading to high blood pressure and inflammation. The body created a solution to this problem with the ACE2 receptor that converts angiotensin-II into angiotensin(1-7), a vasodilator. A vasodilator is a molecule that causes blood vessels to get bigger and allows more blood to pass through. When angiotensin-(1-7) is present in the blood vessel, it prevents the vessel from getting too small and protects the vessel from damage.
SARS CoV-2 Binding on Blood Vessels


The SARS-CoV-2 virus is very similar to the SARS-CoV-1 virus that sparked the SARS outbreak in 2003. Because of this, most of what we know about how SARS-CoV-2 affects the body comes from studies on SARS-CoV-1. When SARS-CoV-1 attaches to the ACE2 receptor, it reduces the number of ACE2 receptors on a blood vessel, which is the same mechanism used by SARS-CoV-2. If SARS-CoV-2 acts like a piece of gum in a lock, then it can quickly reduce the number of ACE2 doors available for normal molecules to act on. Fewer ACE2 receptors means not enough angiotensin(1-7) is being created, which can lead to too much vasoconstriction from the angiotensin-II. This vasoconstriction leads to vessel damage, as seen in figure 3.
The job of red blood cells is to move oxygen to cells around the body. This keeps the cells running smoothly and the body functioning normally. However, when less blood can move throughout the body because of vasoconstriction, less oxygen can get to where it needs to be. This, combined with lung damage, can make a person feel like they are out of breath, and requires more oxygen to be available to the body. Oxygen tanks and ventilators are very good treatments for doing this, as they raise the amount of pure oxygen available to breathe in.
In severe cases, patients can have damage in their brainstem. The brainstem is responsible for the most basic reflexes needed for life: keeping the heart beating, the lungs inhaling and exhaling, and the sensory receptors responding to pain around the body. SARS-CoV-2 can cause encephalitis, inflammation near the region responsible for the gasping reflex in the brainstem. When this reflex is damaged, a patient can have low blood oxygen levels and poor respiratory function without gasping for air as we would expect. Because of this, patients with respiratory problems don’t notice them until they are severe enough to require hospitalization. In other cases, a damaged vessel near the kidneys can lead to renal failure; damage near the liver can lead to chronic liver failure; one near the lungs can cause or worsen damage here, making it harder to breathe. Kumar and his colleagues suggest that this blood vessel damage is the main source of problems caused by SARS-CoV-2 because of the similarity to the earlier virus.
The blood vessel damage caused by the virus can worsen the effects of diseases that a person already has, such as diabetes and obesity. These two diseases can lead to high blood pressure, a symptom that can damage blood vessels and cause clotting, making it harder to move blood around the body. The virus makes these problems worse by adding to the damage, which is why these diseases are two of the biggest risk factors for severe COVID-19 infection.
The extent of damage from COVID-19 is potentially due to how far the virus travels in the body before the immune system starts making antibodies for the virus. However, this is a novel theory and more research is needed to further support it. What we do know is that the risk factors associated with severe COVID-19 infection can exaggerate the known symptoms of COVID-19.
Works Cited
González-Rayas, José Manuel et al. “COVID-19 and ACE -Inhibitors and Angiotensin Receptor Blockers-: The Need to Differentiate Between Early Infection and Acute Lung Injury.” Revista colombiana de cardiología (Bogotá, Colombia : 1989) 27.3 (2020): 129–131. Web.
Kumar, A., Narayan, R. K., Kumari, C., Faiq, M. A., Kulandhasamy, M., Kant, K. & Pareek, V. (2020). SARS-CoV-2 cell entry receptor ACE2 mediated endothelial dysfunction leads to vascular thrombosis in COVID-19 patients. Medical Hypothesis, 145. https://doi.org/10.1016/j.mehy.2020.110320
Wadman, M., Couzin-Frankel, J., Kaiser, J. & Matacic, C. (2020). How does the coronavirus kill? Clinicians trace a ferocious rampage through the body, from brain to toes. ScienceMag.org. doi:10.1126/science.abc3208

I am a graduate student at The University of Texas in Dallas. My primary interest is in neuroscience, but I would try to learn about anything I could if given the opportunity. I want to know why people do what they do and how to use that for policy reform in government and education. I have a dog named Koda and you can catch me going on long walks and sharing my popcorn with him.




Thank you, Audra for making this understandable. I appreciate your efforts.
This made understanding covid so much easier! thank you audra!